

From exploring magic mushrooms to answering COVID-19 questions, here are some of Imperial’s biggest findings this year:
Psilocybin, the psychedelic component of magic mushrooms, was shown in April to increase brain connectivity in people with depression.
Nearly 60 people underwent a clinical study in which they received psilocybin as treatment for depression. Brain scans revealed that the psychedelic had enhanced communication between several regions of the brain. These results were accompanied by subjects’ self-reports that their symptoms had improved, and the effects lasted up to three weeks after the treatment was administered.
“The effect seen with psilocybin […] was not seen with a conventional antidepressant,” explained Professor Robin Carhart-Harris, the paper’s senior author and founder of the Imperial Centre for Psychedelic Research.
Depression often causes the brain to get stuck in certain patterns of activity. Psilocybin seems to expand these rigid brain states, which is something that traditional antidepressants haven’t been able to fully achieve.
 In June, Imperial researchers found that the Omicron variant seems to offer weak protection against future COVID-19 infection, debunking popular beliefs that earlier infections can provide a natural immune boost.
In June, Imperial researchers found that the Omicron variant seems to offer weak protection against future COVID-19 infection, debunking popular beliefs that earlier infections can provide a natural immune boost.
“Getting infected with Omicron does not provide a potent boost to immunity against re-infection with Omicron in the future,” said Professor Rosemary Boyton from the Department of Infectious Disease, lead author of the study. It seems that Omicron is better able to “fly under the radar,” preventing the immune system from remembering and fighting against it in the future.
Professor Danny Altman from Imperial’s Department of Immunology and Inflammation emphasised that the vaccination still offers protection against severe complications of COVID-19. “While our latest findings highlight clear concerns about the nature of Omicron infection, vaccination remains effective against severe disease. Those who are eligible to receive a booster should be encouraged to do so,” he advised.
 Intermittent fasting following nerve injury resulted in enhanced regeneration of neural fibers, according to a study conducted at Imperial this year.
Intermittent fasting following nerve injury resulted in enhanced regeneration of neural fibers, according to a study conducted at Imperial this year.
The researchers put a group of mice on a fasting diet following nerve damage for either 10 days or 30 days, while another group of mice remained on a normal eating schedule after the same injury. Nerve regrowth was around 50% higher in the mice who had fasted. Fasting resulted in the mice’s gut bacteria producing an increased quantity of a metabolite called 3-Indolepropionic acid (IPA), which is necessary for nerve repair.
“There is currently no treatment for people with nerve damage beyond surgical reconstruction, which is only effective in a small percentage of cases,” shared Professor Simone Di Giovanni, the paper’s lead author from Imperial’s Department of Brain Sciences. The team hopes that these findings will be replicated in humans and can potentially serve as a new alternative treatment for nerve injuries.
 The isolation period for COVID-19 changed a number of times throughout the pandemic, and many people were left wondering how long they’re truly infectious for. But an Imperial study announced in August this year may have cracked the code.
The isolation period for COVID-19 changed a number of times throughout the pandemic, and many people were left wondering how long they’re truly infectious for. But an Imperial study announced in August this year may have cracked the code.
After tracking 57 people who tested positive for COVID-19 and exhibited mild symptoms, the researchers found that people were infectious for five days on average. Two-thirds were still infectious five days after symptoms began, but that number dropped to one-fourth after seven days.
“Based on our findings, we recommend that people with COVID-19 isolate for five days after symptoms begin, then use lateral flow tests to safely leave isolation,” said Dr Seran Hakki from Imperial’s National Heart and Lung Institute who was an author of the study. If you do not have access to lateral flow tests, it’s recommended to stay in isolation until receiving negative PCR test results for two consecutive days after the first five days of symptoms.
 Using machine learning technology, researchers at Imperial were able to successfully predict the presence of Alzheimer’s disease in 98% of cases with a single MRI scan of the brain.
Using machine learning technology, researchers at Imperial were able to successfully predict the presence of Alzheimer’s disease in 98% of cases with a single MRI scan of the brain.
This technology, announced in June, would allow for the detection of Alzheimer’s at very early stages of the disease, which is currently quite difficult to do. Having an early diagnosis would give patients time to plan and receive the support that they need well in advance of disease progression.
Lead author Professor Eric Aboagye from Imperial’s Department of Surgery and Cancer explained: “Waiting for a diagnosis can be horrible for patients and their families. Currently no other simple and widely available methods can predict Alzheimer’s disease with this level of accuracy, so our research is an important step forward.”
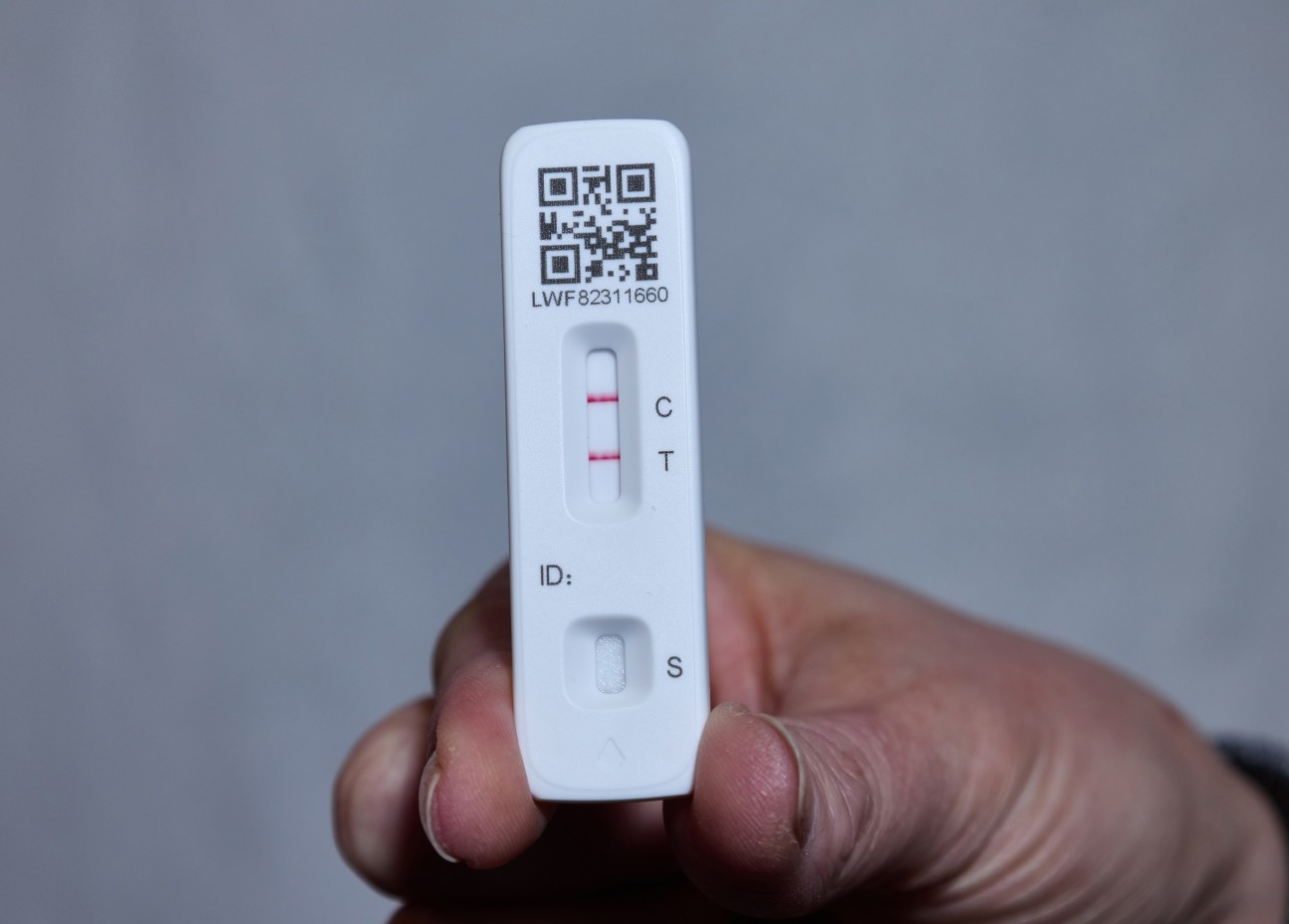 A study conducted by scientists at Imperial, and announced in February, found that lateral flow tests missed 20-29% of positive COVID-19 cases at city testing centers and 81% in university screen testing centers. These false negatives were especially predominant in people not exhibiting any symptoms.
A study conducted by scientists at Imperial, and announced in February, found that lateral flow tests missed 20-29% of positive COVID-19 cases at city testing centers and 81% in university screen testing centers. These false negatives were especially predominant in people not exhibiting any symptoms.
“Lateral flow tests will miss a proportion of people who are infectious, particularly during the early stages of infection,” explained Dr Anika Singanayagam from the Department of Infectious Disease. He stressed that people should understand the limitations of these tests.
An inaccurate test result can provide a false sense of reassurance, which can be problematic in instances where it gives people the ‘green light’ to go visit a person more susceptible to COVID-19. Because of these limitations, Dr Singanayagam recommended that a negative lateral flow test result “should be used in conjunction with other measures such as good ventilation and face masks in such setting to reduce overall risk.”

